Bleeding of a generalized nature with soiling of the operative field and this occurs whenever there is a skin breach. This may be accidental or iatrogenic. Most traumatic injuries with vascular involvement -- self-inflicted, accidental, or done by another person require debridement and, usually, some sort of grafting. Whatever the cause, bleeding causes soiling of the operative field and major vessels may need repair, restoration of continuity, and/or restoration of vascularity to organs of importance. A simple dab applying pressure for a short time takes care of most of the bleeding at capillary and small vessel levels. Again, the body has its hemostatic mechanism that becomes active at this juncture, and this consists of the following --
1. Inward intimal rolling,
2. Constriction of medial muscle fibers, and,
3. Formation of a fibrin-thrombin network where platelets are trapped to form a consolidated clot.
Now, surgically created or traumatic interruption of a wound injures blood vessels in many ways. There can be a total cut, a partial wall disruption, and/or a traumatic contusion leading to endothelial damage with subsequent occlusion by clots forming inside, diameter loss, etc. The colour and the nature of the spurt in the first two instances reveal whether the bleeding is arterial or venous. The volume and the time are taken to indicate whether the bleeding is major or minor and the urgency for control. Contusion of vessels is dangerous as apparently from the outside no damage can be found initially and the physician has to have a high level of suspicion and knowledge of the recognition of such a condition. Furthermore, the extent needed to be resected is difficult to assess and so it is always safe to err and extra-marginal resection on either end when interposition graft is to be considered.
The smaller blood vessels can be clipped or crushed with adequate-sized hemostatic forceps. The prime requirement for vessel surgery is adequate exposure. Only macroscopic vessels having a visible diameter and those that cannot be sacrificed or essentially need revascularization for restoration of circulation, need to be repaired or reconstructed.
Minimizing blood loss is essential as in addition to limiting blood loss, the methods employed also improve visibility thus helping to identify structures. This was realized early. Since antiquity, the use of tourniquets has been recommended to control bleeding. The term "tourniquet" is French, and it is derived from the word "turnere' a vis' meaning turning. The term tourniquet became popular once Jean-Louis Petit presented his theory at the Royal Academy of Paris in 1718. Tourniquet-like devices were common in combats even before and a tight circumferential tie was common to slow retrograde propagation of venom to the central nervous system and heart. Legends say that Shusruta was the first to use it for therapeutic reasons, Galen had reservations, and Ambroise Pare suggested an improvement. Many modifications have been made and of late, the use of tourniquets is advised in modern warfare where foot soldiers are increasingly exposed to mines and incendiary objects. Elastic rubber bandage was first used by Esmarch as a tourniquet in surgery. Tourniquets are mainly used to limit extremity bleeding and slowing, or stoppage of blood loss has been found to save life. Tourniquets in surgery can be used electively or as a help in emergencies. An elective common usage can be seen in orthopedic and plastic surgery. Tourniquets used for the control of bleeding may be a circumferential tie with or without a tightening mechanism or pneumatic. The effectivity depends upon the - 1. Pressure applied - it depends upon the systolic blood pressure of the patient, the width of the cuff, and length of the extremity, and the coefficient of tissue padding (or the nature of tissue surrounding the vessels up to the skin). This is also known as the limb occlusion pressure (LOP). 2. Time - it is advisable to release compression every 10, 15, or 20 minutes and complete the surgery under compression within 2 hours. Studies have shown that 2 hours is the tolerable limit for warm ischemia. It is a well-known fact that tourniquets are not satisfactorily tolerated by small children and the elderly. Nerve injury is a probability and is proportional to the width of the occluding cuff. Some degree of recirculation injury is inevitable and it takes about 40 minutes minimum for normalisation of the metabolic status. However, after consideration, it appears the use of a tourniquet is needed and helps in freeing the compressing hand and fingers. Before the advent of vascular clamps, a tourniquet was the best available method for controlling bleeding, A thorough dissection and debridement of foreign, unhealthy, and unnecessary tissue need to be done immediately followed by passing a loop around the vessel to be reconstructed. The latter should be of supple material, though a wet umbilical tape or thick gauge silk suffices depending on the vessel size. Peri-vascular dissection is difficult in aorto-arteritis and similar inflammatory conditions, where fibrotic tissue is abundant and the finding of a supple arterial segment necessary for anastomosis to the graft is uncertain. Colored elastic tapes are available now which not only loop the concerned vessel but also are atraumatic, colour codes the vessels, and give the surgeon a psychological sense of relief at being in control. Gentle atraumatic retraction of nearby neuro-vascular bundles is also possible. The limbs of the looping material can be brought out of a flexible hollow tube and a Rummel tourniquet is created for ultimate control.
Animal models were necessary and studied extensively from porcine to rat models and across the spectrum of different sizes of vessels. A minimum force has to be applied by the blades of the occluding surfaces of atraumatic forceps. These prevent blood from flowing out through the lumen of a vessel. The size of the vessel matters, and arteries require a greater force due to the increased thickness of the wall. Prevention of endothelial damage and the resultant pathophysiology is the main goal. Atraumatic vascular clamps are designed with similar goals and provide the surgeon with the time and environment for vascular anastomosis. This necessitates a clean bloodless field with adequate exposure and a choice of the right gauge, strength, and material of the suture used. Construction of the clamp is done with a supple but strong and long-lasting material. A lightweight and resilient substance is chosen and multiple catches or stops in the lock are designed to ensure a graduated increase in the closing force when the clamp is used.
Edmund Höpfner (b. 1873) was the first person to use a vascular clamp in Germany in 1903. Such instruments continued to be used till the 60s. Initially, these clamps temporarily occluded arteries and had spring steel jaws that divided in the middle but converged towards the ends, measuring approximately 15 cm in length.
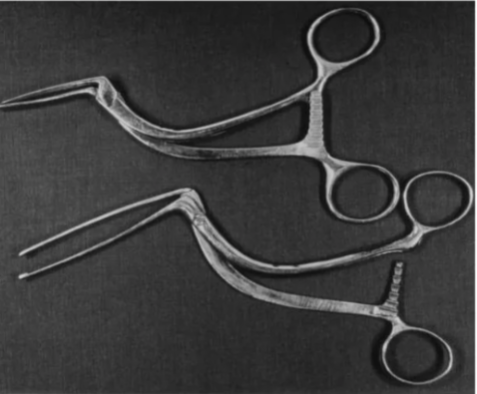
The first tangential occlusion clamp was developed by Friedrich Trendelenburg in 1908 when he established the operative treatment for embolism of the pulmonary artery. This clamp was later modified by A. W. Meyer (1927) and V.P. Satinsky (ca. 1950) to facilitate side to side major vascular anastomosis.
To qualify to be a vascular clamp it has to have the following attributes: -
1. Lightweight,
2. A shank of suitable length with finger rings at one end,
3. The blade is serrated and usually consists of teeth of a particular design for better grip on tissue. The serrations and teeth are designed for a non-bruising secure grip on the occluded vessel and minimize or even prevent endothelial injury. Always the strongest and best stainless material is chosen - stainless steel (high-grade steel), tungsten, plastics, etc.
4. The tip of the blades does not meet at the tip and a graduated force controlled by ratcheted locks applies the pressure on the target vessel once blood stops coming out through the apposed blades, the application of further pressure is stopped. When the tip and the base end of the blades of the forceps meet, the maximum force has been applied.
5. The shape of the shank and curvature or angulation of the blade are designed with a particular task in mind during an operation and also the target organs.
6. When the lumen of a vessel is occluded, it is called a cross-clamp.
7. Tangential clamps are curved, and the size and design chosen to occlude the lumen partially exclude part of the wall of the vessel. Flow across the vessel is maintained through the non-clamped portion.
8. Multiple ratchets with non-return catches are placed in the proximal portion of each blade of a clamp to allow sequential tightening thereby helping in the application of minimum pressure for stopping flow of blood. The principles stated above are true for vascular clamps with a shank. Bulldog and cross-action forceps with spring effect act differently. The spring action is weak and does not injure vessel walls and is designed to prevent bleeding only. The closing clamp pressure depends upon the ratio of the pressure applied to the area of the vessel wall under the blades. This is expressed as g/m² and is a wide range.
Pressure and force are related and the simple conversion rule of Pressure=Force/Area is used with the recent expression of PSI is used as the unit. The flow velocity in the aorta is about 150-175 cm/sec on average. There are many bends and turns in the aorta, and the shearing forces that come with it are not predictable. The arteries gradually taper to progressively smaller sizes as they approach a target organ. Vascular resistance takes into account everything and is a factor in the expressions of pressure in the arteries. The ejectile thrust directly propels the blood column into the arterial system. The measured blood pressure is a combination of vascular resistance and the ejection of the left ventricle. The same pressure that is at the head of the blood column is reflected on the walls and we measure this pressure in the arteries with a sphygmomanometer. Blood pressure is highest at the start of its journey from the heart — when it enters the aorta — and it is lowest at the end of its journey along progressively smaller branches of arteries. The larger the artery greater the bleeding, both in volume and ejection pressure - as high as 500 cm/sec at a region where the left ventricle ejects to the aorta and nearly 0 cm at the capillary level. The magnitude of this pressure might cause slippage of the blades of a clamp in larger vessels if a suitable size is not used even if there are gripping jaw serrations. Hence it is always better to err on the side of safety provided endothelial damage is minimized. Occlusion clamps are stouter in larger vessels. The goal is the cessation of bleeding through the compressed vessel in between the blades of the forceps.
The principles stated above are true for vascular clamps with a shank. Bulldog and cross-action forceps spring effect act differently. The spring action is weak and does not injure vessel walls and is designed to prevent bleeding only. The closing clamp pressure depends upon the ratio of the pressure applied to the area of the vessel wall under the blades. This is expressed as g/m² and is a wide range.
Hemostatic clamps are of two types -- crushing and non-crushing. Common sense says that one cares less about the pressure or force applied and only precisely grasping the tissue is attempted with crushing clamps. However, non-crushing clamps are used when vessel reconstruction is the primary goal. These have serrations and teeth in the blade so that the grip on the tissue is secure and the inner endothelial lining is minimally damaged.
Serrations and teeth in the blade are different. Serrations can be found in crushing clamps also and these have been in vogue since the times of Galen as the crow's beak (Bec de Corbin).
The recent hemostats are commonly associated with the names of Jules-Emile Pean, Spencer-Wells, etc. Alterations to the basic structure are done per the operator's choice and the final shape depends upon the length of the shank, blades, curvature, or the design. Halsted's name is intimately related to mosquito artery forceps - straight or curved. Negus's forceps are exclusively suited to neurosurgery.
The serrations are for ensuring non-slippage and a secure grip. A force of approximately 40 N is applied when the blades of the forceps are placed on the target tissue and the locking mechanism is on.

The serrations are more important in non-crushing atraumatic vascular clamps. Different patterns are there and can be horizontal or transverse, vertical or longitudinal, crisscross, etc. The recent trend is for a lightweight clamp with a thicker blade having either a DeBakey type or a Cooley type of jaw. The DeBakey type has two parallel fine elevated lines of serrations in one blade with a linear groove in-between where the elevation of fine linear serrations of the other blade fits perfectly. The Coley type, on the other hand, sports two parallel rows of fine and elevated serrations just like opposing rails.
These serrations can occupy half the length, full length, a region near the tip, and any length of the shaft. Clamps are named in memory of the person who patented the shape and curvature of the shank and blade, the ratchet locking mechanism, the joint type uniting the two parts, and whether or not finger rings for holding are present or not. Teeth in addition to serrations in the jaws of the blade of a clamp are typically found in forceps dealing with vessels. A variety of patterns and combinations of teeth have been proposed. Earlier slender-jawed forceps with interdigitating teeth were preferred as these were thought to minimize endothelial damage. Also, arterial and even slender venous clamps were separate. Nowadays in most situations, a multipurpose set of different-sized vascular clamps is used with the DeBakey or Cooley serrations. Along with DeBakey and Cooley, the names of Satinsky and Aldo Castaneda should be mentioned. Satinsky became a common name because of the particular angled and curved shape of the blade of a vascular clamp which was a tangential clamp usually used for occluding the left atrial appendage in closed mitral commissurotomy operation. Closed commissurotomy was common even a couple of years back. Castaneda will be remembered for miniaturization and the use of these smaller self-developed clamps for pediatric cardiac corrections.

Vascular clamps -- straight, curved, Satinsky type.

Serrations in the blade

Cooley & DeBakey teeth.
Vascular reconstruction is needed when either there is a partial disruption or a total transection of the vessel. When a portion of the vessel is diseased, then that portion that appears macroscopically unhealthy has to be sacrificed and replaced with an interposition graft with an autologous material if available or a proven bio-acceptable conduit done. The original tissue, if however, can be preserved, should always be used and a double bracing as in Mata's reconstruction is to be done.
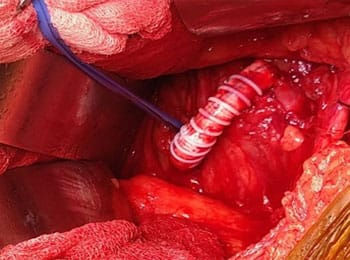
Heparinized or the recent modification of the classical graphite-based heparin bonded shunt (Gott) was used in reconstructive surgery involving large and important vessels where maintenance of cerebral and distal perfusion is necessary. Nowadays, tridodecylmethylaluminium chloride (TDMAC) shunts, which leach heparin slowly and are available commercially in different sizes, are used.
Heparinization is to be done without fail. However, there are some disputes about the dosage. The dosage is reduced amounting to 1 mg/kg of body weight. - Normally 1 IU of heparin is considered equivalent to 1 ml of heparin and a larger dose of 60-80 IU/kg is safe due to the erratic effect of both heparin and the subject. The timing depends upon the surgeon and is usually after major dissections are completed and incidental bleeding controlled, either by fulguration or by ligation. Various and situational doses of heparin is mentioned, and different surgeons have different preferences. Most are happy with the conservative dose of a bolus dose of 5000 International units and the dose is repeated after checking ACT at 10-to-15-minute intervals. An ACT of around 200-250 seconds is recommended and the steady titer is maintained by repeating lower doses intravenously for immediate effect. Where intra-operative measurement of activated clotting time is not there and in emergencies, the 1 mg/kg dose is chosen, and a repetition of half the original dose is injected after one and half hours of a complex procedure because the half-life of elimination of heparin is 1.5 hours.
A clamp of a suitable size and length is chosen. The entire diameter of the collapsible ends (two) of the transected vessel is included within the vascular clamp blades. Tangential clamps are best for holding a part of the wall of a big vessel while allowing a part of the lumen to maintain flow. Tangential clamps are used when the portion of the wall has to be reconstructed, or an end-to-side or side-by-side anastomosis has to be created. When the vessel size is on the smaller side and the transected ends are near, a single tangential clamp will serve the purpose.
The principles of the vascular suture were perfected by Carrel and Guthrie. The inclusion of the endothelial layer in the suture line is necessary and triangulation of the circular conduit helps in the apposition of transected margins of the vessel. Continuous evenly placed sutures with endothelial approximation without purse-string effect give the best result. End-to-end approximation of vessel ends without jeopardizing orientation is mainly sought in single-layer sutures. Margin eversion also is a strategy for not compromising the luminal diameter --- however, at least two layers of sutures, the first layer of horizontal mattress followed by a layer of continuous stitches, are required for this. If interrupted stitches are made, the surgeon has to be very particular about the closeness of the adjacent sutures and does not have the luxury of allowing seepage of blood. The proponents of the interrupted suturing technique state greater strength, no purse string effect, preservation of the suture line lesser bleeding with disruption of a suture, and easier maintenance of orientation. Critics, on the other hand, state that the time taken to complete the anastomosis is longer, the bleeding is less, more knots mean more infection and the continuous suture is better suited for complex composite situations. Continuous whip stitch is more common in cardio-thoracic and vascular practice as a time-saving method and can be easily reinforced by a few interposed interrupted stitches. In expert hands, which usually is the case, there is little difference between the two methods.
Atraumatic non-absorbable or delayed absorbable suture material that incites the least inflammation and thus healing by fibrosis is preferred. The manufacturers have incorporated the suture strand and the needle in such a manner now that eye holes or modifications at the back end of the needle for attaching the suture length to the needle are no longer necessary. Consequently, big needle holes are avoided and the suture with the needle becomes truly minimally invasive being a single unit. There is always a debate about the gauge best suited for vascular repair and it is evident that the gauge depends upon the thickness of the tissue to be pierced, the strength required for maintaining join or anastomotic integrity, and the suture holes it creates during the passage of the material. Thicker suture materials will be preferred for sizably larger repairs, but in vascular reconstructions, smaller gauges and the least reactive substances that produce the smallest holes during passage through the tissue are chosen. Judicious choice of graft material to be sutured for reconstruction is important and it should be remembered that the older PTFE sheets or conduits tended to cut through during the passage of the needle and suture. Considerable bleeding was a complication before these extended needle holes ultimately closed with a platelet-fibrin hemostatic plug.
Monofilament fibers are less likely to get infected. Braided sutures are multifilament, strong, and coated. A braided suture is coated with wax, silicon, fluorocarbon, polytetrafluoroethylene (Teflon), poloxamer 800, etc., to ensure a smooth passage through the tissues to retain strength along with the other qualities of the monofilament materials. However, at the same time, it should be remembered that individual filaments are capable of harbouring spores of apparently innocuous organisms and have the probability to become virulent in the body once the coating breaks down and the nutritional environment is at hand exposing the spores which may become virulent.
Polypropylene is the preferred vascular reconstruction suture material now. A few pediatric cardiac surgeons hypothesize that with the use of non-absorbable substances, the growth potential is hampered. The material of choice for them is polydioxanone (PDS). This material is absorbed late and retains its strength for a long period. However, the use of a thin gauge of polypropylene in corrective infant cardiac surgery has not created a problem with growth, and together with the mental feeling of safety of preservation of the suture lines, polypropylene remains the substance of choice in vascular sutures.
A couple of words about the needles used. The cardio-thoracic & vascular surgeons now usually opt for double-end needled sutures. The suture material and the needles are integrated to minimize Injury. Still, one should remember that the smallest needle with an appropriate-sized thread was used initially. The technology of atraumatic needles and sutures was not known then. Nowadays the needles are made from the highest-grade stainless steel-based alloy. The curvature could be half-circle, less than half-circle, a composite circle with a 3/8th circle near the penetrating end, etc., both according to the ease of penetration of the structure and the preference of the surgeon. Teflon coating is said to impart a black colour to the needle that is supposed to stand out against calcified coronary arteries. The needle points may be conventional, round, round and point, and cutting point. Some have the opinion that the cutting point is more injurious, but for dense tissue or fabric the cutting, spear (diamond or rhomboid, and symmetrically angulated all round in cut section) or wedge (pyramidal or conical, and triangular in cut section) ended, are preferred in vascular reconstruction. A dexterous surgeon can reconstruct whatever the needle curvature point is provided the exposure is right, the needle is manoeuvred along its curvature, and the required instruments are there. Post-repair hemostasis should be meticulous and suture lines must always be covered.
Ramon Castroviejo was an ophthalmologist and was known for corneal transplants. He designed the spring action needle holder for microsurgery. These are versatile instruments and a subtle variation in the finger placement areas allowed a rolling movement of the fingers in the pincer grip. This is the Barraquer variation and makes precise placement of sutures easy by a rolling movement of the fingers used in the pincer grip. The position of the hand remains the same. This needle holder has become very popular with cardio-thoracic & vascular surgeons and is used not only for vascular reconstructions, repairs, and anastomoses but also for surgical sutures of delicate structures in cardiac surgery.

A straight length of the autologous saphenous vein used in a reversed manner is the best conduit material for medium and small vessel replacement and interposition. Dacron and Teflon are the most common biocompatible materials used in vascular surgery. Nowadays thin extended Teflon sheets or conduits with nodes and inter-nodes have come into the market and have become popular. Biocompatible substances can be fabricated, either before or during a procedure as desired by the surgeon, and branches added in accordance. This will be required in major and multiple anastomoses needed in aortic or arch surgery.




Prefabricated valved conduits are available and this is required for the root replacement procedures. Some surgeons even attach a prosthetic valve to a large-diameter biocompatible conduit to save money. Dacron grafts which are crimped and knitted with a double velour surface are usually preferred for the ease of needle passage, fabrication, and suturing. The double-velour surface texturing also helps in neovascularization.
The most popular organ revascularization today is that of the heart. Total arterial revascularization with pedicled arterial conduits is preferred nowadays, especially in the young age group, but the gold standard is an arterial graft, pedicled left internal mammary (LIMA) to left anterior descending artery (LAD) normally, and venous graft to other named coronary vessels. later studies showed better patency rate with side-to-side anastomoses and with the publication and upgrading of internationally accepted guidelines for coronary revascularization, there has been a modification of strategy with a composite LIMA-RIMA Y graft where T, Y (commonest), or I extension of free RIMA with pedicled LIMA is done for sequential anastomoses to diagonal, obtuse marginal (OM), and terminal right coronary (RCA) arteries.
Intestinal revascularization of the superior mesenteric artery relieves thrombotic or embolic obstruction leading to ischemic and digestive problems.

Several vascular anastomoses were strategised for managing impending hepatic failure with spleen-portal hypertension and intractable ascites. Of these the Warren-shunt, where the distal cut end of the splenic vein is anastomosed end-to-side to the top of the left renal vein, became popular and the mesentericocaval H-graft was occasionally practiced. These were major time-consuming procedures and the results were erratic. These are seldom practiced now.
A created arterio-venous fistula is becoming a popular procedure for dialysis access and long-term function can be ensured only when performed by a trained vascular surgeon.
In peripheral vascular surgery, the use of thin ePTFE grafts bonded with heparin is experimentally giving better long-term patency results than autologous vein grafts. Soon commercially prepared and customized by length, diameter, and shape will find a place for those who can afford it.
Porous grafts were notorious for bleeding and heparinization is necessary for handling blood vessels to increase it. The extended poly-fluoroethylene (ePTFE) grafts are not porous but the velour textured dacron grafts are preferred and the pores occluded by impregnation or painting with absorbable collagen or albumin. Some degree of sweating still happens but it is clear and the hematocrit remains the same. Ring-reinforced grafts are favored at the slightest possibility of compression or kink. Whenever possible, auto-grafts are used, and the success of peripheral vascular disease and most cases of coronary revascularization is attributed to the long lengths of properly harvested saphenous veins of the leg and thighs. These free tube autografts, however, become non-viable soon like the Dacron and Teflon grafts and the thrombogenicity is statistically similar and acceptable. Pedicled arterial grafts, like the left or right internal mammary arteries, are popular for coronary revascularization. These grafts can even be lengthened in a T, Y, or I fashion, and similar material is always the first choice. The Japanese favor the pedicled right gastro-epiploic artery for anastomosis to the inferior surface of the heart. The radial artery and the inferior epigastric arteries are harvested as free grafts. Vascularized grafts are also preferred for better acceptability by plastic surgeons while covering complex defects.
Vascular reconstruction requires nit and evenly placed suturing. Sutures may be continuous or interrupted. Continuous suture methods take less time and if evenly placed and with the maintenance of steady pressure hemostasis is better with reduced knot burden. Surgery has to be completed within a reasonable time and reduction of warm and cold ischemia with restoration of physiological function approximating normalcy should always be the goal. Often fibrin or thrombin-based glues are used, and the recent trend has been the usage of polyethylene glycol sealants to reinforce a suture line. However, a proper hemostatic suture line is best achieved with properly taken stitches.

Comments