OEDEMA (Greek - οἴδημα or oidema --> swelling)
Swelling due to the accumulation of fluids in the legs and other parts of the body is known as oedema. This probably is one of the most common complaints in the later age group. Oedema can be of the external (visible) or internal organs and can affect several organs as well as the accumulation of fluids in the body's spaces. The visibility of oedema is best seen in the subcutaneous spaces of the dependent areas. Anasarca refers to generalized subcutaneous oedema of the whole body.
Painful edematous swelling is evident in inflammatory conditions and is maximally surrounding the area injured. The terms exudation and transudation are intimately related and often simple steps help in the differentiation of the two and narrowing the diagnosis. Both consist of a fluid shift from the higher colloid osmotic intravascular environment of blood or lymph to the lower osmotic pressure milieu of the third space.
In transudation, there is a change in the hydrostatic pressure and water with minimum protein and electrolytes are forced across the single-layered endothelial cell lining of capillaries. The increased pressure of blood with constituent haem in the RBCs and proteins and electrolytes forces some fluid out to nearby lowered tissue concentrated spaces through intact capillary and venous wall waves. This fluid will have the least level of proteins and minerals. The fluid is colourless and devoid of cellular elements.
Painless oedema also is found with certain antipsychotic and antihypertensive medicines. Vasodilation of the peripheral vascular wall, reactive in nature, has been cited as a cause.
Exudation consists of leakage through the vessel wall and a disruptive pathology, local or general, has to be there. The colour is darker and the protein content is higher. Purulent or suppurative exudate is one where in addition to macrophages, both alive and dead, are found along with some dead tissue as well. Exudates can primarily be fibrinous, viz., rheumatic carditis, streptococcal throat infection, bacterial pneumonitis, and similar severe injuries.
Oedema with the collection of fluid in third spaces is usually a transudation fluid. The causes are heart failure, liver failure, and kidney failure (better known as the nephrotic syndrome), and caval or major venous obstructions. Thus, facial oedema is a feature of superior vena cava obstruction. Bilateral lower limb oedema usually happens in obstruction at bilateral iliac levels, undue pressure on the iliac veins by a pelvic mass, and in inferior vena cava obstruction, the abdominal veins are prominent with the rostral flow of blood in an attempt at bypassing the obstruction. Ascites are more of a feature when the portal veins are obstructed.
Exudative oedema is found in inflammatory conditions and is either regional or generalized.
Oedema can again be pitting or non-pitting.
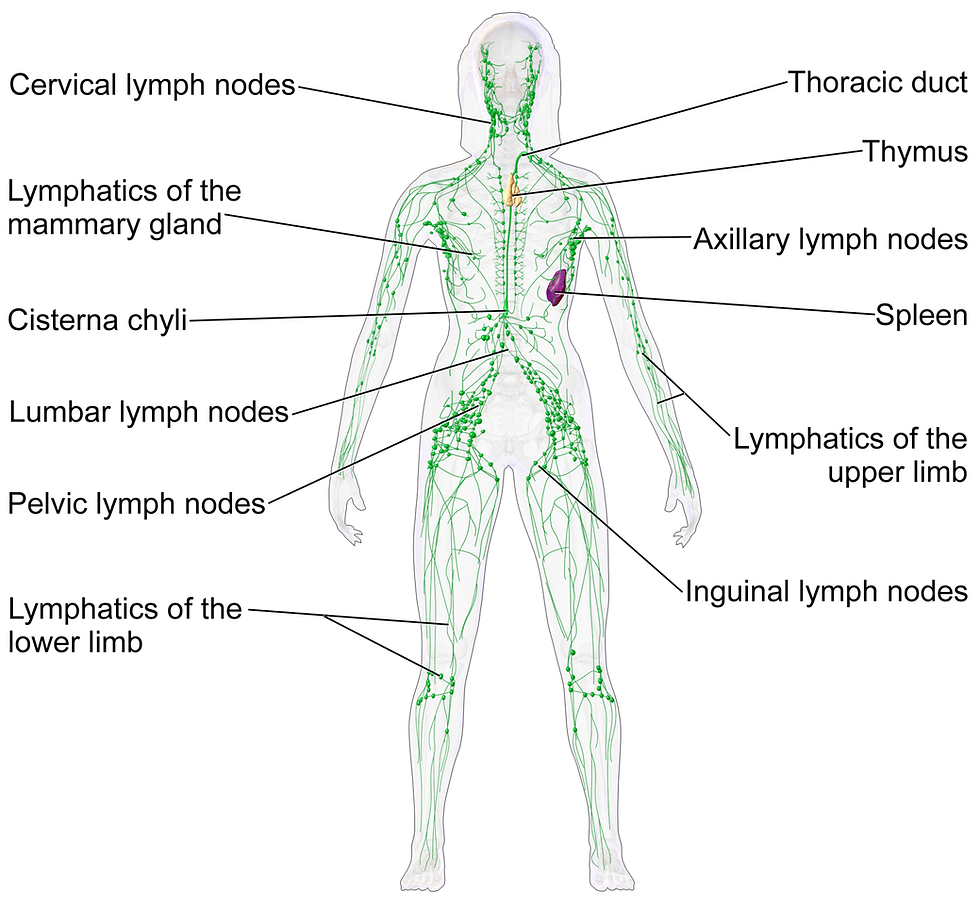
The lymphatic system of the body is unique and removes unwanted and excess fluid from the tissue. There are numerous interconnected nodes and channels, and the final drainage is into the venous system.
Pitting oedema is graded and determined by pit depth (measured visually) and recovery time from grades 0-4. The scale is used to rate the severity and the scores are as follows: Grade 0: No clinical oedema. Grade 1: Slight pitting (2 mm depth) with no visible distortion that rebounds immediately.
Grade 2: Somewhat deeper pit (4 mm) with no readily detectable distortion that reverses in fewer than 15 seconds. Grade 3: Noticeably deep pit (6 mm) with the dependent extremity full and swollen that takes up to 30 seconds to rebound. Grade 4: Very deep pit (8 mm) with the dependent extremity grossly distorted that takes more than 30 seconds to recover.

The time taken for the accumulation of oedema fluid is also important. Rapid collection of third-space edematous fluid occurs with an imbalance in the venous drainage in acute traumatic states, deep venous thrombosis, and cellulitis following a generalized or regional inflammation. When there is a collection in a fascia-localized space, pain is a feature due to pressure on the pain endings. The compartment syndrome of the anterior compartment of the leg of a milder degree is an example of athletes who are forced to do unfamiliar and excessive tasks. In such conditions rest, anti-inflammatory analgesics are the mainstay of treatment. 'Compartment syndrome is a common phenomenon in orthopaedics and early surgical relief may be required to relieve pain and prevent further complications like Volkman's ischemic contracture, neural damage from ischemia, and DVT. Stitch removal in oedematous tissue, fasciotomy, and lay opening of a wound is to be done without delay as the situation demands. In DVT, the posterior compartment of the leg where the calf muscles are housed is typically affected. Dorsiflexion of the foot at the ankle joint causes pain in the calf. This is known as the Homans sign (John Homans, 1941). This is associated with warmth and tenderness to pressure in most cases.
The following points are important and worth mentioning: --
1. Gradual build-up of the transudative oedema fluid occurs mainly in the failure of the heart, kidneys, and liver. There is a gross increase in intravascular hydrostatic pressure together with the inability of these vital organs to handle the electrolytes. Such oedema is usually bilateral. Unilateral oedema commonly occurs in –
1. Mastectomy following carcinoma of the breast.
2. Axillary vein thrombosis. 3. Tumour pressing upon the iliac vein of one side.
Transudative tissue oedema is an important sign of heart failure. The compromised heart and the circulatory system fail to handle the tissue effectively. Pitting oedema results and the fluid in the interspaces of the loose tissue organs like the lung may lead to cough, shortness of breath, and even frank pink-frothy sputum. This is also known as 'pulmonary oedema'. Oedems in kidney diseases are obviously from the tissues an inadequate clearance of the fluid from the system along with wastes for very many causes.
Oedema in hepatic failure is both cytotoxic and vasogenic. Cerebral encephalopathy, ascites, loss of memory, and confusional states are commoner with hepatic failure, and ammonia along with ammoniacal products like glutamine have been anecdotally blamed. Ascites in liver failure are more likely in the various forms and stages of cirrhosis where the pressure in the veins associated with the portal system is high.
Lymphedema is a situation where there is proximal obstruction of a significant draining node or a group of nodes. Carcinoma, irradiation, and radical surgery with nodal clearance as the management is the most typical cause. Parasitic infection with filaria leads to a bilateral leg swelling which is likely to become non-pitting and huge assuming a gigantic size, in the long run, to be aptly termed ‘elephantiasis’.
The causes of primary and hereditary lymphedema are different and, in most cases, according to some, the deficiency of GATA proteins is a transcription factor critical for embryonic development, maintenance, and functionality of stem cells involved in blood and lymph-forming tissue. There are familial or sporadic inactivating mutations in one of the two GATA genes, inherited from each parent, leading to a deficiency of the GATA proteins. In other situations, like the Milroy disease, the gene regulating the vascular endothelial growth factor receptor 3 (VEGRF-3) is affected. In any case, the role of tyrosine kinase has been noticed. Primary and hereditary lymphedema. as of now, is believed to be an autosomal dominant condition and is also known as haploinsufficiency where the equal genetic contribution of both parents is necessary.
Primary lymphedema is usually rare and associated with several syndromes like Turner/Noonan syndromes, Klippel-Trenaunay-Weber syndrome, yellow nail syndrome, lymphedema-distichiasis syndrome, etc.
Primary lymphedema can again be hereditary, and three types have been recognized -- Type I- familial genetic disorders (VEGFR3 gene) like the Milroy disease/Hereditary lymphedema type I/Congenital familial lymphedema/Nonne-Milroy lymphedema. This rare type of lymphedema is apparent at birth and may be unilateral or bilateral, affecting genitalia or the face. Type II- where the symptoms develop around puberty or shortly thereafter. This is also called the Meige disease or lymphedema praecox. A commoner type where the voice box is affected as well. Type III- the 3rd variety is lymphedema tarda occurring after the age of 35 years. In women the lower limbs are most affected and though the lower limbs, the other areas are also involved with the sluggish drainage of lymphatic fluid.
There are other forms of lymphedema, and they can be visually unpleasant as well. Lymphedema ptosis is one condition where the upper eyelids are affected to give a drooping look. Of the other rare conditions come the distichiasis-lymphedema syndrome,

and the yellow nail syndrome.
In the former, the only expression may be a double row of eyelids. Bilateral leg oedema, ptosis, photophobia and astigmatism, cleft palate, and cysts in the spinal cord, with or without multi-system affection of organs due to improper drainage of lymphatic fluid may occur in this pathology during puberty or thereabout. There may even be a cardiac defect. Yellow nail syndrome is also a rare condition in which the nails become curved, thick, and fail to grow. The tough curved nil may be separated from the thicker cuticular skin around, and the nail, grotesquely shaped, can fall off. Pleural effusion with attendant respiratory symptoms and ascites is often associated.

Lymphatic diseases are suspected in non-pitting swellings, warty excrescences, non-healing ulcers in swollen skin regions, and a peau d’orange appearance with non-pitting swollen skin. Radical mastectomy with axillary clearance is the most common cause of non-pitting unilateral upper limbs. There is a condition often wrongly diagnosed as lymphedema and that is lipedema. It is important to understand that lymphedema resulting from insufficiency or a block in the drainage system will incite a progressive and recurrent inflammatory reaction. At times this can lead to a secondary malignancy. Another condition is the mistake made while recognizing a region affected by lipodermatosclerosis in varicose veins.
Patients want relief from the swelling. Management can be subdivided into-
1. a part managing transudations, 2. an effort to control exudations, and 3. managing non-pitting oedema.
Transudations are easier to manage. In most cases, especially in posture and drug-related situations, a simple elevation of the edematous part is all that is necessary. The addition of a diuretic hastens the procedure provided the patient is hemodynamically stable. Diuresis also plays a major part in getting rid of the extra water in circulation with a low ejection of the heart in heart failure. Thus, a combination of inotropes which increases the ejection qualities of the heart along with a diuretic is recommended to upgrade renal perfusion and excrete the excess water.
The exudative collection is usually inflammatory in origin. The presence of injurious irritant materials and malignancy is more likely to induce fluid collection in the pleural, peritoneal, and joint spaces. Malignancy is more likely to induce hemorrhagic fluid. Ascites may be a feature. Management in such situations consists of eradication and control of these conditions.
Lymphoedema leads to non-pitting oedema. Management is difficult and not always rewarding. Diuretics usually have no role. The mainstay of management includes regular massaging and retrograde compression aimed at improving vicarious lymph drainage.
Surgery involves a massive plastic procedure where a reduction in the fibrous tissue and remodelling of excess skin is done to revert to the original body shape. However, the surgery is done rarely, and the results are not gratifying.
The commonest cause of non-pitting lymphatic oedema in India, bilateral or unilateral lower limb solid non-pitting oedema, is due to an Aedes mosquito bite causing filariasis. There are medicines to kill the offending pathogens, but the tissue changes are difficult to manage. Identifying a major draining lymphatic vessel is a surgical challenge after a lymphangiography with a dye and thereafter, an even more difficult lymphovenous anastomosis has to be done. The results, if at all successful, are dubious and hence, though theoretically sound, fell into disrepute.
A chylous pleural collection will require conservative management first with the abstinence of oral foods (especially fat-containing) and intravenous fluids. A non-residual diet containing medium-chain fats only has been found to help in such situations. Octreotide (somatostatin) may have a role in the reduction of the amount of fluid. Surgery is considered the last option after failure of other conservative regimes, A thoracotomy after a fatty meal containing cream 3-6 hours before induction. A tracer like Evan's blue or more specifically Isosulphan blue is injected in the web spaces in between the toes of the feet with the hope the colored tracer in the lymphatic fluid will ooze out at the region of the breach. If the point or region of a breach in the lymphatic channel is not recognized, a mass ligation of the para-aortic adventitious tissue on the right side at the retro-aortic and retro-caval pericardiophrenic junction is done. A shunt with the peritoneum may relieve some cases, of not responding to conventional methods.
To conclude, it has to be mentioned that oedema remains an important observation and sign. Many reasons can be attributed to oedema, but one important factor is whether it is pitting or solid. The common causes should be explored first before the diagnosis is made.
Commentaires