When we started revascularizing blocked coronary arteries, we noticed that in most cases, the target vessels had lost suppleness and had degenerative fatty lesions in the walls which considerably reduced the flow. Further, a large vessel that needed exploration showed a yellow atheromatous core having a variable consistency, hard in places soft pultaceous within layers of the media and an irregular intima. A picture on Wikipedia showing discoloured separated serum convinced clinicians of the seriousness of the condition.

Observation of such lesions and the fact that such lesions are more likely to be found in individuals who are prone to consume food unlimited amounts of fatty material convinced physicians that fatty food was not good for health. The idea that saturated fats cause heart disease, called the diet-heart hypothesis, was introduced in the 1950s, based on weak, associational evidence. It has been well documented since then that certain individuals with, e.g., type 2 diabetes, hypertension, obesity, chronic obstructive lung disorder (COPD), etc, are particularly susceptible to the deleterious vasculopathy effects of fatty material and may accelerate untoward terminal events.
Fats are a group of substances that dissolve in organic solvents and are not mixed with water. Fat that naturally comes with the food we consume is better known as dietary fat. The forms of dietary fat that are known are --:
1. Saturated fat, (SFA),
2. Monounsaturated fat, (MUFA),
3. Polyunsaturated fat, (PUFA),
4. Trans-fat, and
5. Cholesterol.
Fatty acids are a straight chain of an even number of carbon atoms, with hydrogen atoms and a carboxyl group at one end. The long chain of the fatty acid mainly contains methyl groups joined by a single bond. The presence of a double bond between these methyl moieties makes a fatty acid unsaturated and the number of double bonds also decides whether a fatty acid is mono-unsaturated or poly-unsaturated. The length of the chain and the position of double bonds also determine the nomenclature. Cis- is the common isomeric form but there may be a transformation to a trans-isomeric form in certain situations. Only two fatty acids are known to be essential for humans: alpha-linolenic acid (an omega-3 fatty acid) and linoleic acid (an omega-6 fatty acid). These cannot be formed by the body due to the absence of the desaturase enzymes. The essential fatty acids, in addition to the usual fatty acid function, are also precursors to vitamins, cofactors, and derivatives, including prostaglandins, leukotrienes, thromboxanes, lipoxins, etc. As only two were essential, initially these were called "vitamin F" and later an essential fatty acid due to, the chemistry.
There are some confusing terms about fatty substances when investigation reports are read. Simple interpretation consists in agreeing to the fact that fats are a large chain molecular conglomeration of triglycerides which are stored as adipose tissue in the body. Fat in medical terms is called a 'lipid' and prevents heat loss due to a subcutaneous positioning, protects vital organs by being placed around them and is the major source of stored energy for the body. Esterification with glycerol forms glycerides and in lipid molecules three fatty acid molecules are involved, hence the term 'triglyceride. In adipose tissue, the fatty material is stored as triglycerides and large lipid conjugates. Triglycerides are smaller-sized lipids and are found in measurable quantities in the bloodstream. Similarly, cholesterol is a waxy or greasy substance and forms the basis of the structure of gonadal hormones mainly and the bulk of the brain matter. Cholesterols are considered essential molecules that are synthesized in the body in bulk and need little external dietary supplementation to bolster the blood level. There is a range with a safe upper limit and the state of hypercholesterolemia is genetic. Fat saturation depends upon the presence of paired covalent bonds in the molecule and the number of unpairing determines the nature of unsaturation. The facts worth remembering are that: -
1. Saturated fats are bad for vascular health and arteriopathies like diabetes or hypertension leading to stiffening and narrowing of the arterial wall, and endothelial erosion. and medial deposition of atheromatous fatty material.
2. Polyunsaturated fat is potentially better and unsaturated fats are good for cardiovascular health.
3. The trans isomeric form of fats, or the trans-fats, are not good for health, and hence physicians always advise staying away from commercially baked and fried foods, and shortenings. margarine, refrigerated biscuit material and rolls, ice cream, pizza, etc.

The main difference in the physical state of fatty substances is the presence or the absence of covalent bonds between the carbon atoms in the lipid moieties. The accompanying chart is a fair representation of lipids in different physical forms, e.g., oily liquid or solidified at lower temperatures.
When considering the investigation report about lipid levels in blood some confusing terms are encountered, such as lipoproteins, chylomicrons, apo-A, apo-B, etc. are all lipoproteins and the nanometric size increases as the density of the lipoprotein decreases. Low-density lipoproteins, chylomicrons, and their remnants are all atherogenic and not good for
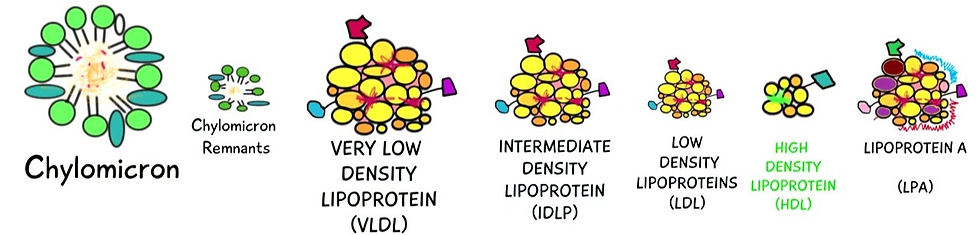

Only the high-density lipoproteins (HDL) are anti-atherogenic and they form the smallest portion of the transporting lipoproteins. Density and size are inversely proportional, and the less dense and larger lipoproteins are all atherogenic. Low-density lipoproteins, chylomicrons, and their remnants are not good for cardiovascular health.
There are two pathways for lipoprotein assimilation in the body - the exogenous pathway for dietary fats, and an endogenous hepatic pathway where ultimately cholesterol is formed and added to the lipoproteins to form chylomicrons. Simplified, the dietary fats are mainly consumed as fatty acids and on entering the enterocytes, they are esterified to triglycerides. This is the hydrophobic inner core of fatty acids and triglycerol, and to this,e.g. the outer layer of a hydrophilic outer monolayer of phospholipids with cholesterol is added. Apoproteins are next attached at specific sites to act as ligands for certain enzymes. Chylomicrons thus formed enter the lacteals of the villi of the intestinal wall, and via the lymphatic system, they ultimately enter the bloodstream.
In the bloodstream, these fatty substances have unique important functions --
They transport and deliver fat-soluble essential vitamins like A, D, E, and K to the target tissue.
Most are stored in adipose tissue as fatty acids and triglycerides and are an important source of energy at stressful times.
Triglycerides store unused calories and provide the body with energy while cholesterol is used to build cells and certain hormones.
Adipose tissue, both subcutaneous and around organs, provides a vital cushion from blunt injuries.
Chylomicrons also called ultra-low-density lipoproteins (ULDL), are mainly responsible for the delivery of dietary cholesterol to the liver. These are the largest of all lipoproteins, have a specific affinity for apo-B48 as a ligand, and allow emulsification in the bloodstream.
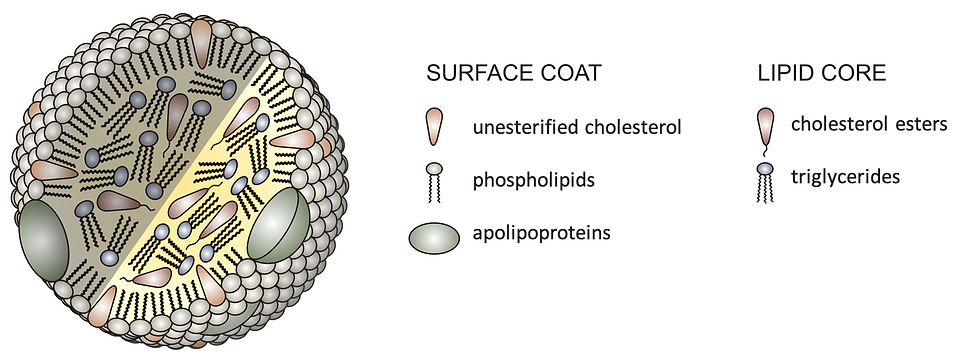
The diagram is a fair representation of the chylomicron structure and shows how fatty material insoluble in water is transported in the blood. The core contains mainly water-insoluble fatty acids such as triglycerides and redundant cholesteryl esters. The mantle is hydrophilic allowing transport in the blood. This hydrophilic nature is due to an orientation of the water-miscible end of the phospholipid molecule to the exterior. Phospholipids are numerous on the surface, the other molecules being free cholesterols and a few apolipoproteins. Both are interspersed scantily within the numerous phospholipid molecules. The apolipoproteins are amphipathic and essentially synthesized and added to a lipoprotein moiety for acting as ligands for the action of the enzyme lipoprotein-lipase.
Each lipoprotein class is heterogeneous in its protein constituents. Nine distinct apolipoproteins have been separated and described. Most investigators group the apolipoproteins into five families (designated apo A, apo B, apo C, apo D, and apo E) based on their chemical, immunologic, and metabolic characteristics. Apo A refers to the apolipoproteins (apo A-I and apo A-II) that are primarily, but not exclusively, found in HDL. A third member of the apo A family, apo A-IV, is a minor component of chylomicrons. Apo B is the major apoprotein of LDL but also comprises about 35% of VLDL protein. There are two forms of apo B: a large form called apo B-100 found in LDL and a smaller form called apo B-48 produced mainly in the intestine. Apo C represents a group of apoproteins (apo C-I, apo C-II, apo C-III) that were originally described as major components of VLDL but that are also present as minor components in HDL. Apo D is a minor component of HDL. Apo E is a major component of VLDL and a minor one of HDL. The apolipoproteins serve both structural and functional roles. Some apoproteins are ligands for specific cell surface receptors, e.g., apo B-100 and apo E for the LDL (or apo B/E) receptor. Others are cofactors for enzymes, e.g., apo C-II is a necessary activating cofactor for lipoprotein lipase.
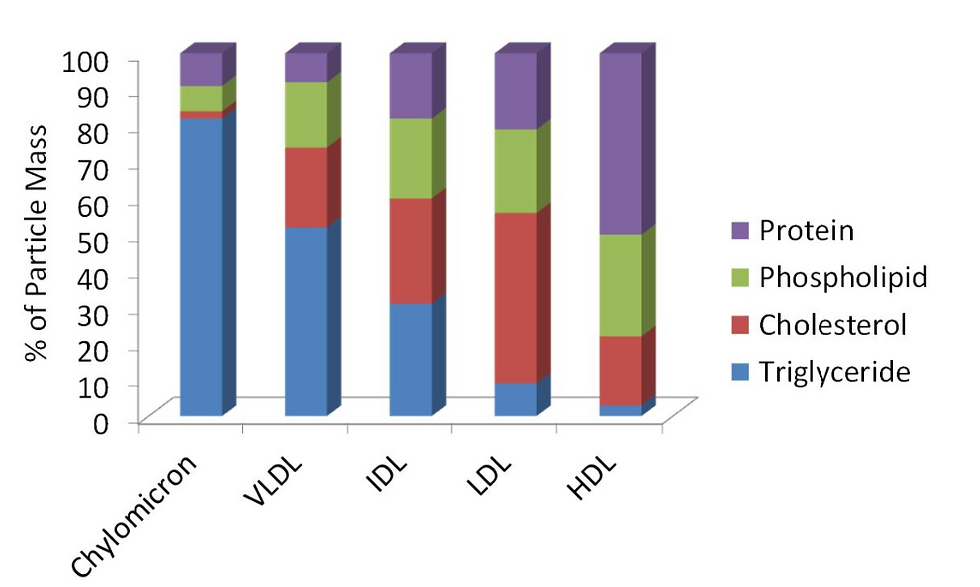
This figure gives an idea of the comparative constituents of the various types of lipoproteins. Hence, we see that triglyceride levels progressively increase with the size of the lipoproteins. The free cholesterol content is highest in the LDL fraction.
As said before triglycerides provide the maximal amount of energy of the major food sources. During the feasting stage, triglycerides are taken up and stored in the adipose tissue as fats. Fasting elicits a different type of action. Stored triglycerides in the adipose tissue are mobilized and metabolized in the Hmg-CoA pathway and the energy thus released is utilized. The process is slower but eminently suited for hibernation or similar events.
Thus, clinically we often get individuals with normal looks where the lipid levels in the blood are severely deranged. Peri-orbital xanthelasma skin patches may be the only indication of high lipoprotein levels. Conventionally the body mass index is calculated and any value, when assessing a subject, > 30 is taken as obese. Obesity is a condition affecting mainly affluent people in society, especially those who have a sedentary lifestyle. The lipid profile in obese subjects is faulty. However, subjects having lipedema will have an improper distribution of fat and are not always, strictly speaking, obese. High LDL and cholesterol levels in a blood panel screen alert the physician and today's food habits with lack of exercise, and further aggravate the existing vasculopathy. Dyslipidemia is usually polygenic and multifactorial, lacking a single underlying mechanism, and can often be approached based on individual abnormal components. Endocrine and/or nephrologic referral is often required for unmasking hitherto asymptomatic preventable states which makes the subject more vulnerable to the ill effects of high lipid levels.
A new entity has come to light when looking in depth at the exponential rise in coronary and other vascular problems in the South Asian population. Dyslipidemia, in the form of exceedingly high VLDL level, is common but the BMI never is >= 30. However, the proportion of adipose tissue to muscles and others is paradoxically altered. Phenotypically such individuals may have a normal appearance and commonly they are thin but with a protruding belly. These states have been variously named normal weight obesity, metabolic obesity, metabolically unhealthy non-obese, skinny fat, and sarcopenic obesity in the elderly, but the name 'Thin obese' became popular. screening for this condition is troublesome as the available procedures today, viz., the Dual absorption x-ray, whole-body CT scan or even better MRI scan, are costly, voluminous, cumbersome, and not suited for community screens. The presence of high amounts of atherogenic lipoproteins makes these individuals particularly prone to coronary heart and peripheral arterial disease. Adding to these is the unusually high resistance of Insulin to adipose tissue. Thus, adult adult-onset diabetes or type II diabetes is a common association and adds to the complexity of the problem. Still, the measurement of BMI, assessing skin fold thickness, and measurement of waist circumference constitute the rapid and acceptable methods of obesity and big body weight determination and physiological ranges are set for reference.

A lipid screen has become routine for the evaluation of a middle-aged person to find out a hidden problem. The popularity of a lipid panel in the middle aged has even led to its inclusion in cardiovascular health check-up corporate packages. The typical lipid panel gives the following values --
Serum total cholesterol
serum HDL cholesterol
Total cholesterol/HDL cholesterol ratio
Serum triglycerides
Serum Phospholipids
Further electrophoretic fractionation is done to determine the percentage of
(a) Chylomicrons,
(b) LDL,
(c) VLDL, and
(d) HDL.
As cholesterol comes from other sources as well, forming the basic framework for the molecular structure of certain essential steroids and also forms the bulk of neuronal brain tissue, a ratio of HDL and VLDL is given with the report so that the risk of atherogenicity can be predicted. The higher the ratio greater the risk and care providers are happy with a ratio below 5:1 and a ratio of 3.5:1 and below is considered reasonably good.
Some authorities think that the levels of Apo-A1 and Apo-B with a ratio are more sensitive and specific for cardiovascular health. A range of 0.19 to 2.60 with a median of 0.52 is found in normo-lipidemic profiles. An increment of 20% greater vasculogenic risk is to be considered if the value exceeds 0.9.
However, other than predicting the state of vascular pathology for cardiovascular health, a lipid profile cannot differentiate between the different types of hyperlipidemic states. Thus a hyperlipidemic individual is only identified when a deranged value is found in a routine screen. The time of appearance of periorbital xanthelasma patches cannot be predicted and such individuals do not look like obese subjects with several comorbidities. Other than predicting the vasculogenic risk, a check of the lipid profile is necessary, once deranged values are detected, to prevent further progression once a pathology sets in. One has to understand that there are many forms of hyperlipidemia designated according to the fraction of lipoprotein elevated in the blood, e.g., hypercholesterolemia, hypertriglyceridemia, and hyperlipoproteinemia. hyperchylomicronemia or familial hyperlipoproteinemia type 1 (HLP-1), etc. Hyperlipidemia can be primary or secondary. In the primary forms, there usually is a genetic abnormality that interferes with lipoprotein lipase, lysosomal lipase, and the function of apoproteins. Some primary hyperlipidemias can have polygenic reasons and the basis can also be mixed in some cases. The association between type II diabetes and hyperuricemia is not uncommon. The types are -
Type I,
Type II, (sub-grouped as IIa and IIb),
Type III,
Type IV, and
Type V.
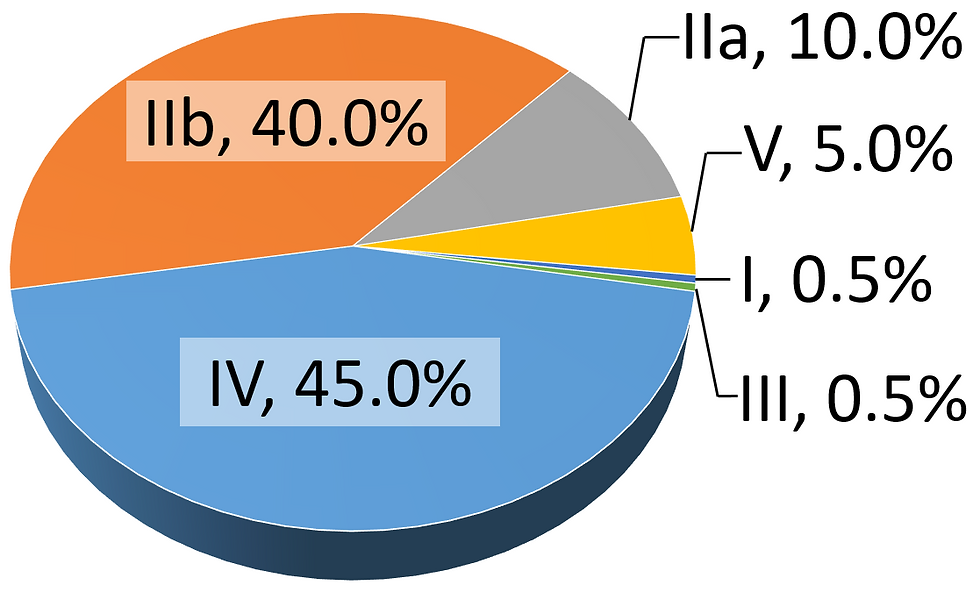
The figure here shows the relative incidence of the various types of genetically inherited lipoproteinemia.
In addition, there are rare forms of familial hyper-alpha-lipoproteinemia and polygenic hypercholesterolemia. The secondary or acquired forms are usually caused by the following diseases -
Type II diabetes,
Hypertension,
Chronic renal diseases and renal failure,
pancreatitis,
Various thyroid diseases,
Certain drugs,
A sedentary life with a lack of adequate exercise,
Fast food and an eating habit where plenty of saturated and trans fat is taken,
Alcohol abuse,
A few rare endocrine and metabolic disorders.
The association of a hyperlipidemic state in the blood further increases the vasculogenic risk and makes these patients susceptible to cardiac and cerebral morbidities culminating, in most instances, in sudden death.
To avoid such morbid conditions brought on by high levels of fatty substances in blood modern physicians advise the following measures -
avoidance of fatty and fast food including fries, cheese and other whole milk products like butter and ghee,
avoidance of any fat and lards or vegetable oils that solidify on cooling.
paradoxically peanut butter is vico-elastic liquid, and all nuts are good for health, packed with plenty of vitamins and minerals, especially selenium along with the base calory,
fish fat contains an abundance of the poly-unsaturated essential omega 3 & 6 fatty acids good for cardiovascular health and should be consumed,
avoidance of refrigerated dough for biscuits and cookies,
alcohol to be taken in moderation,
smoking in any form is bad,
regular exercise and physical activity.
active weight regulation,
stress relief,
statins after dinner and at night before sleep.
In addition, the cardiologist advises a low-salt diet to prevent heart failure. Several dietary options have been devised to lower or normalize the serum lipoprotein level. Though a few plans are practised diligently by some motivated groups, none have been universally accepted.
Fat degradation and metabolic release of energy occur in starvation or similar states. The histopathological examination has shown that fatty tissue in the body also called the adipose tissue, is found extensively at subcutaneous planes and in and around certain organs. In both situations, that minimises the jarring effects of a blunt force. The unitary lipid-laden cells are called the adipocytes and where they are found in abundance they are loosely held together by strands and fascia. Fatty infiltration leads to weakness and organ dysfunction. Recent research, mainly from the '90s has revealed some interesting facts which were not known before. First, Leptins was discovered about 36m years back. Leptins are produced primarily by the adipocytes in white adipose tissue. Here it plays important physiological roles indirectly (primarily via the nervous system) and directly (by the adipocytokine action). It was theorised then that these leptins were responsible for the fine balance and neural control for releasing energy from the triglyceride-rich adipocyte cells and the uptake of triglyceride and fatty acid into the adipocytes for energy storage. Adipocytes like other cells had membrane-bound cytoplasm and intra-cytoplasmic inclusions. The size and the colour depended on the lipid droplet and the number of other intracytoplasmic inclusions like the mitochondria, Golgi bodies, nucleus, and endoplasmic reticulum. The lipid droplet contained triglycerides, fatty acids, cholesteryl esters, and a few cholesterols. Earlier majority white and few areas of brown adipocytes, e.g., the neck and the thorax, were identified. The white adipocytes with large lipid droplets were the real energy storage cells and the brown adipocytes were broken down first during energy requirement as the mitochondrial content was high. Recent data suggest two more varieties --
The beige adipocytes, which appear to be an intermediary between the white and brown adipocytes, and the
The pink adipocytes - though no evidence still exists in humans, almost instantaneous production of energy-rich, proteinaceous, vitamin & mineral-containing, and basic immunogenic milk from the mammary glands made researchers investigate further. In animal models, the spontaneous transformation of certain adipocytes with a pinkish hue was found to produce intracellular milk droplets.

Recent findings also attribute some special metabolic functions to the adipocytes, e.g, --
Adipose tissue secretes a variety of effectors, including exosomes, miRNA, lipids, inflammatory cytokines, and peptide hormones that act in both paracrine and endocrine capacities,
Insulin sensitivity and glucose metabolism.

Adipose tissue now is considered a separate organ with very unique functions. The major functions revolve around the parameters shown in the figure and in addition to other energy release functions during hibernation and starvation states.
In conclusion, we have to remember that fat and cholesterol are important for the body, but there is a limit to the consumption of fat-containing and fried food. The risk of cardiovascular health proportionately increases with age and though knowledge about the progressive vasculogenic pathophysiology is there, the timing of future catastrophic events is not possible. Some vegetable-derived saturated fats used in cooking may be good for the brain and other organs, but they are highly atherogenic. Thus, the right advice is still elusive.
Comments